Which weight-loss drug is more effective?




People lost substantially more weight when they took Eli Lilly’s diabetes drug Mounjaro than Novo Nordisk’s Ozempic, with roughly the same side effects, drop-out rate and benefit for diabetes, according to the first major head-to-head study.
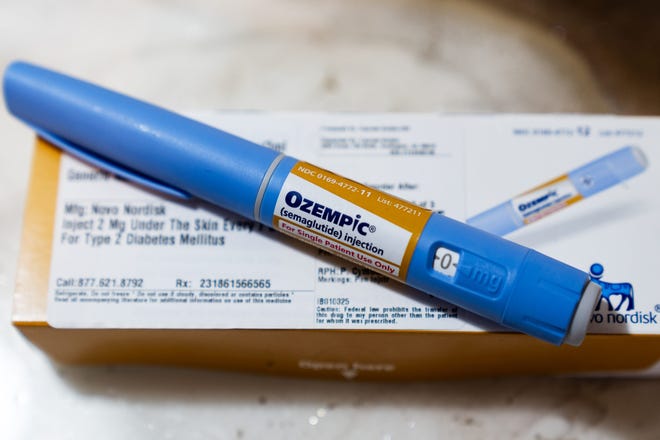
Both drugs are in the same class, known as GLP-1s, but Lilly’s drug, tirzepatide, sold under the brand names Mounjaro for diabetes and Zepbound for weight loss, includes a second action that seems to boost its effectiveness. Separate studies had suggested tirzepatide led to more weight loss than semaglutide, which Novo Nordisk sells as Ozempic, for diabetes and, Wegovy, at a higher dose, for weight loss.
The new study, published Monday in JAMA Internal Medicine, compared data on more than 18,000 patients who began taking one of the two medications between May 2022 and September 2023. The study relied on electronic health records from Truveta, a collective of health systems across the country with access to data on more than 100 million patients.
At the time, tirzepatide hadn’t yet been approved for weight loss, just diabetes, so the study looked only at people who had prescriptions for the two drugs for type 2 diabetes, although not everyone had the disease.
By November of last year, more than half of the people on both medications ‒ 56% of those taking tirzepatide and 53% of those taking semaglutide ‒ had stopped taking them. Although the study didn’t confirm a reason, many have previously reported side effects from the drugs, typically gastrointestinal, including vomiting and nausea.
The study didn’t report whether the people who dropped out regained any weight they lost. Previous research has shown that so-called yo-yo dieting can cause more health problems than simply carrying extra pounds.
But GLP-1s are by far the most effective and safest class of weight drugs ever developed. More than 70% of Americans meet the medical definition of overweight and 40% of obesity.
“As we’ve tracked GLP-1 use over the last couple of years we’ve just seen these dramatic increases of use,” said Tricia Rodriguez, who led the study for Truveta Research, with both drugs, “really revolutioning the treatment of both diabetes and obesity.”
Clear winner? Not so fast, Novo says
Novo Nordisk disputed the study’s conclusion.
“The ideal way to compare two treatments is an adequately powered head-to-head randomized clinical trial (RCT) in obesity. Currently, no head-to-head trials have been completed comparing tirzepatide and semaglutide 2.4 mg,” the company said in a statement sent by Allison Schneider, the company’s director of media relations & issues management.
The 2.4 mg dosage is the highest of semaglutide typically used for weight loss. The highest dose used to address diabetes is lower, so the dosage used by people in the study, which focused on people diagnosed with diabetes, would have been below the optimal dose for weight loss.
For tirzepatide, the highest dosage is the same, whether for weight loss or diabetes.
Specific takeaways from the study
People taking tirzepatide were nearly twice as likely to lose 5% of their body weight as those taking semaglutide; 2.5-times as likely to lose 10% of their body weight; and more than 3 times as likely to lose 15% of their body weight, the study showed.
After three months on each drug, those taking tirzepatide had lost an average of about 6%, while those taking semaglutide had lost just under 4%. At six months, those on tirzepatide had lost 10% while those on semaglutide had lost 6%. And at a year, those on tirzepatide had lost 15% of their body weight, compared to 8% for those on semaglutide.
As has been found in other studies, people with diabetes lost less weight on the medications than people who had obesity but not diabetes.
Among the 18,386 people studied, 70% were female, 77% were white, 11% were Black and just over half had type 2 diabetes. Their average body-mass index was 39 and their average age was 52. More than one in five had also been diagnosed with depression.
Obesity, diabetes and depression often overlap, in part because they are all so common, in part because medications for mental health conditions are associated with weight gain and diabetes onset, and in part because they contribute to each other, said Dr. Katherine Saunders, an obesity medicine expert at Weill Cornell Medicine in New York.
“Obesity and diabetes can worsen depression, and depression can worsen obesity and diabetes,” she said.
Why they’re dropping out
Many patients stop taking these extremely effective medications because of side effects and access issues, say doctors who prescribe them.
The side effects can typically be controlled with adequate medical oversight and proper ramping up of the medication, experts say.
“Patients require more than a prescription for a GLP-1 medication in the last few minutes of a busy appointment,” said Saunders, also co-founder of Intellihealth, which provides medical obesity treatment.
Personalized care, time and “tons of education and support” are needed to help people start and stick to these medications, she said.

Both drugs are meant to be taken step-wise, started at a low dose and advanced slowly to higher doses. If a patient cannot tolerate a higher dose, they are typically left at a lower one indefinitely or until side effects lessen, said Dr. Fatima Cody Stanford, an obesity medicine specialist at Massachusetts General Hospital in Boston.
Cody Stanford said her only patients who discontinue a GLP-1 for medical reasons are the 1 in 1,000 or so who develop pancreatitis, a painful inflammation of the pancreas, and the 15% or so who don’t see any substantial weight loss after a significant period of time.
For those people, Cody Stanford said, she often has to convince them the drug others describe as a “miracle” simply isn’t going to work for them.
“This isn’t a ‘try harder’ situation,” she said. “If it works, it works.”
Cost and access problems
A much more common reason for discontinuing a GLP-1, Cody Stanford said, is an inability to get access to a reliable and consistent supply.
Both drugs have been hard to access because of supply issues.
Novo Nordisk says it has provided Wegovy to more than 1 million Americans since 2021, and the highest dose strengths of 1.7 mg and 2.4 mg are now fully available, “which aligns to our goal of doing our best to ensure existing patients have continuity of care as they dose escalate per the label,” according to a company statement.
“At this time, we can’t speculate when Wegovy® will become fully available at all dose strengths but we are doing everything we can to build manufacturing capacity and supply to meet patient needs,” the statement continued.
Supply updates are available at WegovySupply.com.
Lilly did not respond to a request for comment, but has struggled to keep up with demand for tirzepatide, particularly since it was approved for weight loss under the brand name Zepbound.
For her patients, Fatima Cody Stanford said she now has been able to access Novo’s semaglutide, but not Lilly’s tirzepatide.
Both drugs cost about $1,000 a month for the highest dose, with Wegovy, Novo Nordisk’s semaglutide formulation for weight loss, costing more than Ozempic, its diabetes drug, because the highest dose is higher.

Cody Stanford said the high price and access problems mean people who need the medications most have the hardest time accessing them.
Most of the study participants were middle-class white women ‒ with those prescribed tirzepatide even more likely to be white and female, Rodriguez said. There’s a difference between the patients on tirzepatide and those on semaglutide and some patients can’t access either one, she said.
Black, Hispanic and Native women have the highest rates of obesity and diabetes, but typically don’t get coverage for GLP-1s. “There’s a mismatch in who gets coverage with these more novel therapies and who doesn’t,” Cody Stanford said.
Source link
